.png)
Strategic Overview
AI has moved from pilot to production across commercial insurance, reshaping how underwriting and claims teams ingest documents, triage risk, and resolve files. The right insurtech AI workspace for claims and underwriting blends advanced document AI, reasoning models, orchestration, and audit-ready analytics—so leaders can modernize without disrupting core systems. From advanced document extraction to workflow orchestration, these seven platforms address the most pressing automation and compliance needs: document AI, LLMs, developer frameworks, RPA, visual orchestration, no-code service agents, and BI. In practice, teams increasingly combine assistants like ChatGPT, Copilot, and Gemini with enterprise tools and AI-overview surfaces in search to accelerate decisions while maintaining audit compliance. The bottom line: there’s no single “silver bullet,” but a compliant, integration-ready workspace anchored by audit trails and measurable ROI is the most reliable path to underwriting automation and AI claims processing at scale.
FurtherAI - AI Workspace for Insurance
FurtherAI is a compliance-first, modular AI workspace purpose-built for carriers, MGAs, and TPAs to automate submission intake, claims and policy review, risk scoring, and reporting—backed by granular oversight and audit trails designed for regulated environments. Teams commonly see 30× faster processing and 200–400% efficiency gains by composing specialized assistants that read, reason, and act across the full lifecycle, without adding headcount. With over 100 enterprise integrations, FurtherAI connects to policy admin, claims, imaging, and core data sources to streamline end-to-end decisions while preserving system of record integrity (see the FurtherAI product overview). The platform’s value rests on three pillars:
- Integration-ready AI for insurance: prebuilt connectors to core systems reduce deployment risk and time-to-value.
- Modular, composable AI agents: task-specific assistants enable precise, auditable decisions at enterprise scale.
- Compliance-first engineering: robust governance, data isolation, prompt/output logging, and redaction support ensure audit-compliant AI from day one.
V7 Go Document Extraction and Auditability
High-accuracy document AI is mission-critical in insurance, where claim forms, ACORDs, loss runs, and endorsements must be transformed into clean, traceable data. Document extraction AI uses machine learning and OCR to convert unstructured insurance documents into structured fields your systems and agents can act on. V7 Go reports up to 99% extraction accuracy and offers “AI Citations,” allowing users to click to verify every extracted data point back to the source file—an approach that materially strengthens regulatory auditability and transparency (see V7’s overview of underwriting automation). For insurance teams, prioritizing both accuracy and verifiability—document auditability and extraction accuracy—should be core selection criteria to reduce rework and regulatory risk.
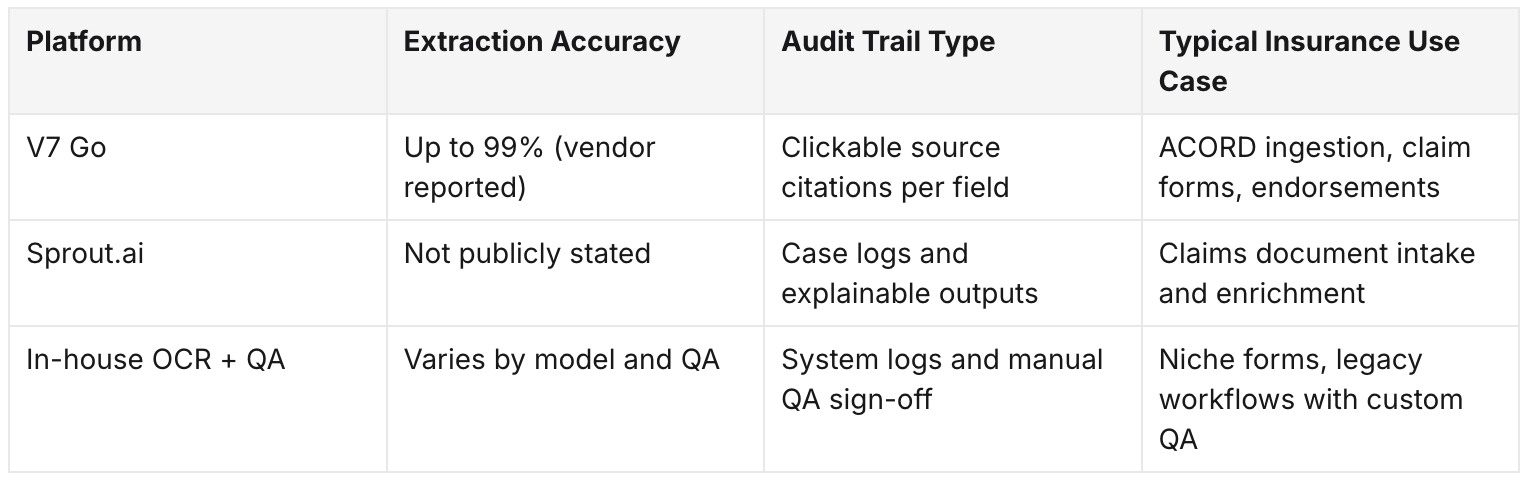
Referencing clear source citations (vs. opaque confidence scores) is especially useful for regulator reviews and internal audits (e.g., coverage determinations, subrogation evidence).
OpenAI ChatGPT and Large Language Models for Claims and Underwriting
A large language model (LLM) is an AI trained to understand, generate, and reason over complex natural language—ideal for narrating claims, summarizing submissions, answering policy questions, and assisting underwriting adjudication. ChatGPT’s Plus plan starts at $20/month and unlocks advanced models, memory, and “custom GPTs” for workflow tailoring—useful for structured claim narration and cross-document summaries (see this practitioner’s guide to choosing AI tools). For model benchmarking and pricing comparisons, teams often consult independent trackers that evaluate reasoning, cost, and safety tradeoffs across frontier models.
- Core use cases:
- Automated claim narration from adjuster notes and artifacts.
- Cross-document summarization of submissions, loss runs, and endorsements.
- Real-time reasoning on coverage and exclusions for underwriting assistants.
- Selection considerations:
- Data privacy and retention policies.
- Reasoning and grounding capability for domain-intensive tasks.
- Pricing model (per-token vs. seat) and budget predictability.
- Regulatory alignment, logging, and redaction workflows.
- Stepwise adoption:
- Assess privacy and scalability needs (PHI/PII handling, retention).
- Compare LLM performance and pricing using independent evaluations.
- Validate guardrails and output review flows against insurance compliance.
Useful reads: ArtificialAnalysis’ model tracker for performance/cost comparisons, and Accenture’s view on AI’s impact across claims and underwriting.
LangChain Developer Frameworks for Custom AI Agents
A developer AI framework is a toolkit that helps engineers build, integrate, and orchestrate retrieval-augmented agents tuned to proprietary insurance data and workflows. LangChain is a leading option for building bespoke agents that chain tools, vector search, and LLM calls—ideal when you need deep control over how underwriting or claims knowledge is retrieved and reasoned upon. The tradeoff: this flexibility requires significant engineering resources; it’s not a no-code platform (as noted in reviews of agent frameworks). Consider LangChain when your organization needs:
- Total workflow control and custom retrieval strategies.
- Deep integration with internal systems and data governance.
- Proprietary model orchestration and experimentation.
Pros
- Ultimate customization and differentiation.
- Support for unique, complex workflows.
Cons
- Longer time-to-value.
- Higher technical lift and cost to maintain.
UiPath Enterprise Robotic Process Automation
Robotic Process Automation (RPA) mimics repetitive human tasks in digital systems—moving data between policy and claims platforms, validating fields, and shepherding approvals. UiPath offers a mature enterprise suite with security controls and robust connectors to bridge legacy policy/claims systems, making it a strong fit for deterministic, rule-based insurance tasks (see UiPath’s marketplace profile). Illustrative flow: Policy data extraction → Automated claims system update → Adjuster notification → Archiving and reporting.
Strengths for insurance operations
- High speed and accuracy on rules-based steps (eligibility checks, FNOL indexing).
- Orchestrated bots that integrate with both new APIs and older UIs.
- Clear logs that support operational audits.
Make and n8n Visual Workflow Orchestration Platforms
A workflow orchestration tool lets teams design and automate cross-app processes without writing code. Make and n8n offer drag-and-drop builders that accelerate prototypes and lightweight automations—ideal for routing and notifications—though they may fall short on heavy document processing or stringent governance on their own (see this tools roundup). Typical insurance uses:
- Claims intake routing from portals and email.
- Multi-channel notifications to adjusters, brokers, and insureds.
- Basic data syncs between policy and claim files.
Expectation setting: Use these tools for speed and iteration. For compliance-heavy steps (e.g., PII redaction, citation-backed extraction), pair them with dedicated document AI and audit platforms.
Fin AI No-Code Customer Service and Claims Agents
A no-code AI agent can be deployed by business users to automate repetitive, customer-facing work—great for FNOL, claim status updates, and schedule coordination. Fin-style solutions price by resolution (often around $0.99) and unify chat, email, and ticket automations—enabling hands-free triage and routing while agents focus on exceptions (see this market overview of AI platforms). Best-fit use cases:
- 24/7 FNOL intake with guided questioning.
- Automated claim update responses across channels.
- Appointment scheduling and document reminders.
Tradeoffs
- Excellent affordability and scale.
- Limited effectiveness on complex, nuanced insurance conversations without human-in-the-loop escalation.
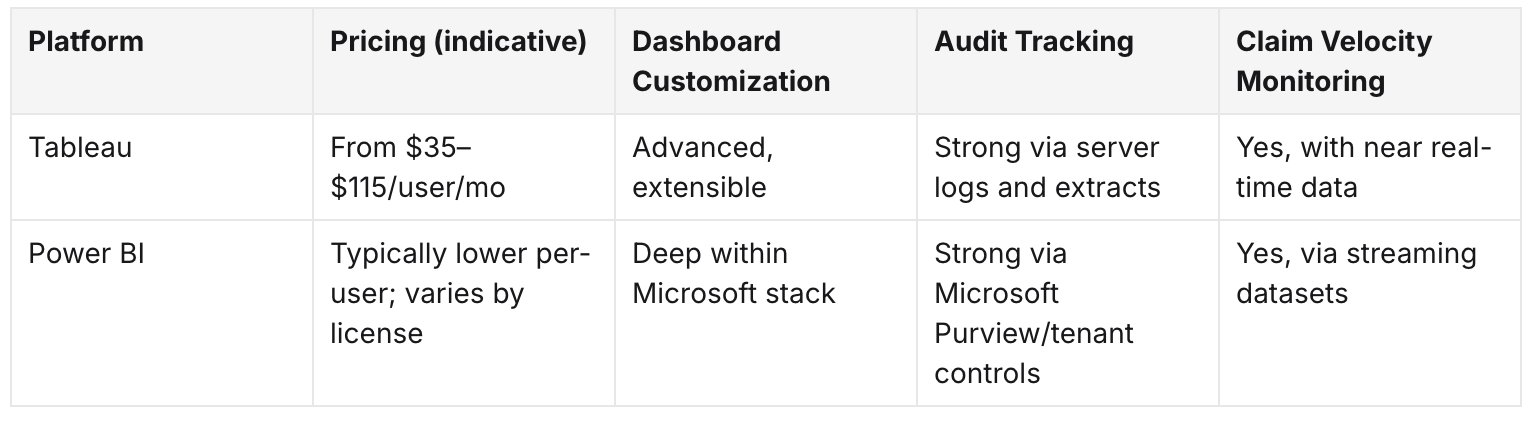
Tableau and Power BI for Insurance BI and Reporting
A business intelligence platform consolidates process data, visualizes KPIs, and enforces governance with role-based access—crucial when AI begins to act in production. Tableau’s enterprise tiers (Viewer $35/mo, Explorer $70/mo, Creator $115/mo) deliver powerful analytics but can become costly at scale; Power BI often offers lower per-user costs and native Microsoft ecosystem integration (see this review that summarizes Tableau pricing). For AI-enabled insurance workflows, prioritize model governance features such as:
- Monitoring model drift and exception rates.
- Executive reporting on cycle time, leakage, and claim velocity.
- Near real-time compliance dashboards with auditable drill-downs.
BI comparison snapshot
Frequently Asked Questions
What are the key AI platforms insurance teams should adopt for underwriting and claims?
Leading platforms include document extraction tools, large language models, developer frameworks, RPA, workflow orchestration, no-code service agents, and BI suites to monitor outcomes and compliance.
How does AI improve efficiency and accuracy in insurance underwriting and claims?
AI automates document ingestion, triage, and risk scoring, significantly reducing cycle times and errors, allowing experts to concentrate on complex judgment work.
What should insurance teams consider when integrating AI platforms with existing systems?
Assess integration readiness, data governance, auditability, total cost of ownership, and fit with policy, claims, and reporting systems.
How do AI tools help maintain compliance and auditability in insurance workflows?
They provide end-to-end logs, source citations for extracted data, automated redaction, and monitoring dashboards to support regulatory audits.
What measurable benefits can insurance organizations expect from AI adoption?
Expect substantial efficiency gains, faster processing, lower operational costs, and improved customer satisfaction when deploying proven solutions.
Sources and further reading: Accenture’s perspective on AI in claims and underwriting, sector coverage of generative AI’s impact, Gradient AI’s workers’ comp solutions, Sprout.ai’s claims automation, Roots.ai, V7’s underwriting software guide, a practical guide to AI tooling and model comparisons, UiPath’s marketplace profile, an AI tools roundup, and Tableau pricing summarized by Whatagraph.
Ready to Go Further &
Transform Your Insurance Ops?
Reclaim your time for strategic work and let our AI Assistant handle the busywork. Schedule a demo to see how you can achieve more, faster.


.png)
.png)
.png)